At the Laboklin expert panels, renowned experts provide answers to questions on exciting and current topics. We have summarised the highlights from the panel on CKD for you. The invited experts were PD Dr. Roswitha Dorsch from (senior lecturer for urology and nephrology at LMU Munich, Germany), PD Dr. Petra Kölle (senior lecturer for animal nutrition at LMU Munich, Germany), Prof. Dr.Rafael Nickel (Dipl. ECVS, Evidensia Veterinary Clinic Norderstedt and Associate Professor for urology at FU Berlin, Germany), and Dr. Ariane Schweig-hauser (Dipl. ACVIM and ECVIM-CA (Internal Medicine), specialised in nephrology and extracorporeal blood purification procedures at Vetsuisse University of Bern, Switzerland).
Dr Dorsch kicks things off by explaining how chronic kidney disease (CKD) is defined. It is characterised by a long-term reduction in kidney function and/or changes in kidney structure, affecting one or both kidneys. CKD is defined as lasting more than 3 months, which is the time it can take for kidneys to recover from an acute kidney injury.
The cause of CKD often remains unknown, but sometimes metabolic or congenital diseases, as well as dietary factors, are identified during the diagnostic process. Ureteral obstructions, chronic bacterial infections, and infectious diseases may also be involved. Notably, cats with CKD often show higher levels of antibodies against leptospires compared to healthy cats. Therefore, testing for leptospirosis using tests such as the MAT and urine PCR may be considered for free-range cats that hunt mice.
According to Dr. Schweighauser, acute renal injury will always leave the kidneys with a certain amount of residual damage. Therefore, lifelong monitoring of kidney function is essential to detect complications such as hypertension and possible progression to
CKD. This enables timely intervention and adjustment of treatment.
PD Dr Kölle emphasises that avoiding excessive protein and phosphate is an important measure to minimise the risk for CKD development and progression. She advises feeding a diet composed for senior pets to dogs and cats once they reach the age of 8 years. As a general rule, excess protein in a cat’s diet, often resulting from expensive, meat-heavy food, should be avoided.
Prof Dr Nickel points out that mechanical outflow obstructions can lead to a CKD in the long term or enhance its progression. When asked whether he considered the calcium oxalate stones often found in the context of CKD to be the cause or consequence, he replied that the primary disease is localised in the tubules. In the first instance, it is probably the result of CKD however, its stage also triggers further damage.
Dr Schweighauser confirms the common impression that the prognosis of CKD in dogs is generally worse than in cats. However, the IRIS stage at the time of the initial diagnosis also has a major impact on the prognosis. Survival times are significantly better if the disease is detected in stages 1 or 2. It also matters whether the CKD is static or progressive at the time of assessment.
Dr Dorsch discusses the laboratory parameters that are important when assessing kidney function. Creatinine, urea, and SDMA levels are elevated when the filtration capacity of the kidneys is compromised. It is crucial not to base the diagnosis on a single blood test but to confirm the persistence of azotaemia through repeated measurements. Newer diagnostic parameters include FGF-23 (fibroblast growth factor 23) and indoxyl sulphate.
Dr Schweighauser adds: ‘SDMA is more meaningful than creatinine in emaciated patients, in patients with muscle atrophy and in small dogs such as Yorkshire terriers. However, it is subject to a high biological-analytical variance with daily fluctuations.
If SDMA alone is elevated, she recommends retesting after 3 months and at the same time points out that SDMA can also be elevated in other diseases (e.g., lymphoma) and in young animals.
FGF-23 is a protein that is involved in phosphate homeostasis. Among other things, it is activated by increased phosphate concentrations in the blood. This reaction occurs when total body phosphate is increased even if blood phosphate levels remain within the reference range. FGF-23 is therefore crucial for the early detection of such dysregulation. Additionally, high FGF-23 concentrations are correlated with the prognosis and progression of CKD. With respect to treatment, increased FGF-23 indicates the need to reduce phosphate intake. Dr Kölle and Dr Dorsch agree that FGF-23 can be used to monitor the success of a renal diet.
Another ‘new’ parameter in the laboratory is indoxyl sulphate, a uraemic toxin produced from indole. Elevated concentrations damage the tubule cells of the kidneys and favour the progression of CKD. Indoxyl sulphate is prognostically relevant.
Urinalysis is an essential part of the diagnostic work-up of kidney diseases. Urine specific gravity (USG) provides information about the concentration capacity of the kidneys. It is measured using a refractometer. Urine is inadequately concentrated if the USG is <1.035 in cats and <1.030 in dogs. Dr. Schweighauser explains that kidney disease should be considered with persistently low USG, especially if azotaemia is present. However, USG results should always be correlated with other test results as USG varies greatly depending on the hydration status of a patient or recent water intake. Hyposthenic urine (USG < 1.008), on the other hand, is not consistent with kidney disease.
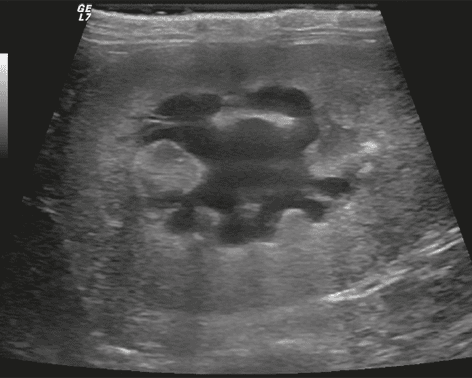
At this point, Prof. Nickel emphasises that sonography must be an integral part of the examination to detect drainage disorders, evidence of pyelonephritis or neoplasia, and, in younger animals in particular, dysplasia and other congenital diseases. Sonography can be a valuable tool for detection of morphological changes in early kidney disease. In addition, it often is helpful when it comes to differentiation of acute from chronic disease.

When asked about the importance of urinary sediment examinations, Prof. Nickel explains that he looks for calcium oxalate crystals in cats, especially in the presence of renal mineralisation or uroliths. Normally, these crystals are easily recognisable in the urine and allow conclusions to be drawn about the type of stones present. However, the majority of cats with calcium oxalate urolithiasis unfortunately do not have crystals in their urine. Dr Schweighauser adds that this is the case because as soon as a urolith has formed the crystals tend to bind to the stone rather than appear within the urine. If calcium oxalate is suspected, she likes to determine the concentration of ionised calcium in the blood. Both emphasise how important it is to examine the urine while it is fresh, as artefacts can quickly develop after a short standing time.
Dr Kölle is asked to provide guidance on the ingredients and their information on the feed. She confirms that it is often difficult to assess the information on protein and phosphate because the necessary calorie intake must be included in the ration calculation. In principle, it can be assumed that veterinary diets are optimally formulated. If such a diet is not desired by the pet owner or is not accepted by the patient, an over-the-counter kidney diet is certainly preferable to conventional feed, even if these often do not fulfil the requirements of a veterinary diet. As an alternative from her own kitchen, she recommends pork as the meat with the lowest phosphate content, preferably high in fat, along with carbohydrates, a phosphate-free vitamin-mineral mixture, and a source of essential fatty acids, such as hemp oil. However, an initial professional ration calculation is important to avoid feeding errors. Regarding the introduction of a kidney diet, she refers to studies showing that it can take up to 30 days for a cat, in particular, to become accustomed to a new food. During the familiarisation phase, toppings such as a little tuna or warming up the food can help increase acceptance.
Can dry food also be fed?
Dr Kölle explains that cats naturally drink little and do not adequately compensate for water losses on their own. If only dry food is fed, water intake must be actively encouraged. Suggestions for this include: using drinking fountains, placing multiple water bowls around the home, preferring shallow glass bowls, ensuring water bowls are never next to the litter box or near the food bowl, and enriching the water with flavours.
When asked when a renal diet should be started, Dr Schweighauser explains that it makes sense to start early (IRIS stage 2 at the latest). A change in diet is easier while patients do not suffer from nausea and lack of appetite, and an early reduction in FGF-23 appears to slow progression. Determining FGF-23 levels in the blood can help decide whether phosphate reduction is needed and to what extent. However, reducing phosphate too early and strictly can lead to opposite effects and the development of hypercalcaemia in cats.
On the subject of subcutaneous infusions, Dr Dorsch explains that these can improve the quality of life for cats with CKD. However, not every cat with CKD needs to be infused. As long as the hydration status is good, this treatment is not necessary. Subcutaneous infusions are useful from IRIS stage 3 and in patients with vomiting, diarrhoea, or loss of appetite. Dr Dorsch recommends buffered solutions (Sterofundin or Ringer’s lactate) at a dosage of 75-100 ml two to three times a week. Volume overloads should be avoided at all costs.
When asked about treatment with adsorbers such as Porus One®, Dr Dorsch discusses a study conducted in-house. Porus One® is a carbon-based adsorber designed to capture uraemic toxins, including indole in the intestine, which reduces its absorption into the blood. This, in turn, leads to lower synthesis of indoxyl sulphate in the liver. The study involved 19 cats with CKD: 10 received the preparation while 9 served as the control group. After 6 months, the indoxyl sulphate concentrations in the blood of the cats in the experimental group were significantly lower than those in the control group.
When asked about when phosphate binders should be used, Dr Kölle explains that they are only necessary if the dietary feed is not accepted and/or if the phosphate concentration or FGF-23 levels in the blood cannot be sufficiently reduced.
She also highlights the risk of phosphate deficiency if uncontrolled dosing occurs.
ACE inhibitors and angiotensin receptor blockers (ARBs) are primarily recommended to reduce proteinuria, according to Dr Schweighauser. ARBs can also be used to control hypertension in cats with CKD. There is evidence suggesting that these medications may offer additional benefits by mitigating the effects of the renin angiotensin aldosterone system (RAAS). Reducing intraglomerular pressure can help counteract glomerular fibrosis. However, the use of ACE inhibitors and ARBs is contraindicated in unstable and dehydrated patients, as well as those with advanced CKD. From IRIS stage 3 onwards, these preparations should no longer be used without caution.
The next question is directed to Prof Nickel: What should be done about uroliths in the ureter, and when? Early diagnosis can be challenging. At the onset of obstruction, there may be colicky pain that is not always recognised. Symptoms of ureteral obstruction are often non-specific and, in many cases, are only identified late. It is not uncommon for significant dilation of the renal pelvis and lasting kidney damage to have already occurred. The prognosis is significantly better with early detection.
Therapeutically, it may be possible to flush out small calculi using induced diuresis and an alphasympatholytic agent (e.g. alfuzosin), thereby relieving the obstruction. Surgical approaches to stone removal are also possible but carry the risk of scar stricture formation. If the calculus is located in the lower third of the ureter, it can be removed by shortening and reimplanting the ureter. Alternatively, a subcutaneously placed bypass can be used.
Dr Schweighauser does not consider dialysis a realistic long-term therapy for patients with CKD. It is a good option for patients with acute kidney failure and can be used in chronic disease to bridge acute episodes with the aim of achieving a stable condition. However, she emphasises that despite intensive therapy, the blood values after the acute phase will generally be worse than before, as a new injury will have further damaged the kidneys.
The final question is about dental health and CKD. Dr Schweighauser believes that regular dental care is essential due to the impact of chronic inflammatory processes and bacterial infections on kidney health, even if it requires anaesthesia. She recommends hospitalisation with intravenous infusion 24 hours before and after the procedure. She emphasises the importance of good intraoperative monitoring, including blood pressure measurement, reducing narcotics through the use of regional anaesthesia, and avoiding drugs such as NSAIDs in connection with anaesthesia. It is also important to check kidney values before and after anaesthesia, as well as a few days later.
Dr. Jennifer von Luckner