Pemphigus foliaceus (PF) is the most common autoimmune skin disease in dogs and cats. The primary lesion is a pustule that results from desquamation of keratinocytes (acantholysis) due to antibody-mediated destruction of desmosomes. The distribution pattern of lesions is highly suggestive of PF, especially in the early stages, but further investigation is always needed to confirm the diagnosis.
Introduction
The epidermis is composed of a multilayered squamous epithelium. The individual keratinocytes are connected to each other by desmosomes. These cell adhesion molecules are composed of various proteins, such as desmocollin and desmoglein. Autoantibodies directed against these structures lead to the destruction of the desmosomes and subsequently to acantholysis and the formation of subcorneal pustules. In most cases, the disease develops spontaneously/idiopathically, but there are some factors that can trigger an episode. These are primarily medications such as various antibiotics, but also topical ectoparasiticides and cimetidine in cats. However, only some of the patients experience remission after discontinuing the suspected medications. Increased exposure to ultraviolet light worsens the symptoms. An association between canine atopic dermatitis and the development of PF is also being discussed. However, due to the high prevalence of allergies in dogs and the concurrent use of various medications in allergy sufferers, it is difficult to establish a clear link between the occurrence of PF.

Clinical signs
The clinical picture is similar in all species and is often symmetrical. The skin changes are due to the formation of pustules as a result of acantholysis. However, these pustules are very fragile and are therefore not always recognised during dermatological examination. They rupture easily and quickly develop into erosions and crusts, which over time can merge into thick yellowish plaques. In dogs, the pattern of spread extends from the face, especially the dorsal parts of the nasal planum (Fig. 2), the bridge of the nose, the pinnae (especially on the inside), and periocularly over the neck, abdomen, and back to the paws and pads. The skin in the inguinal region is also often affected.

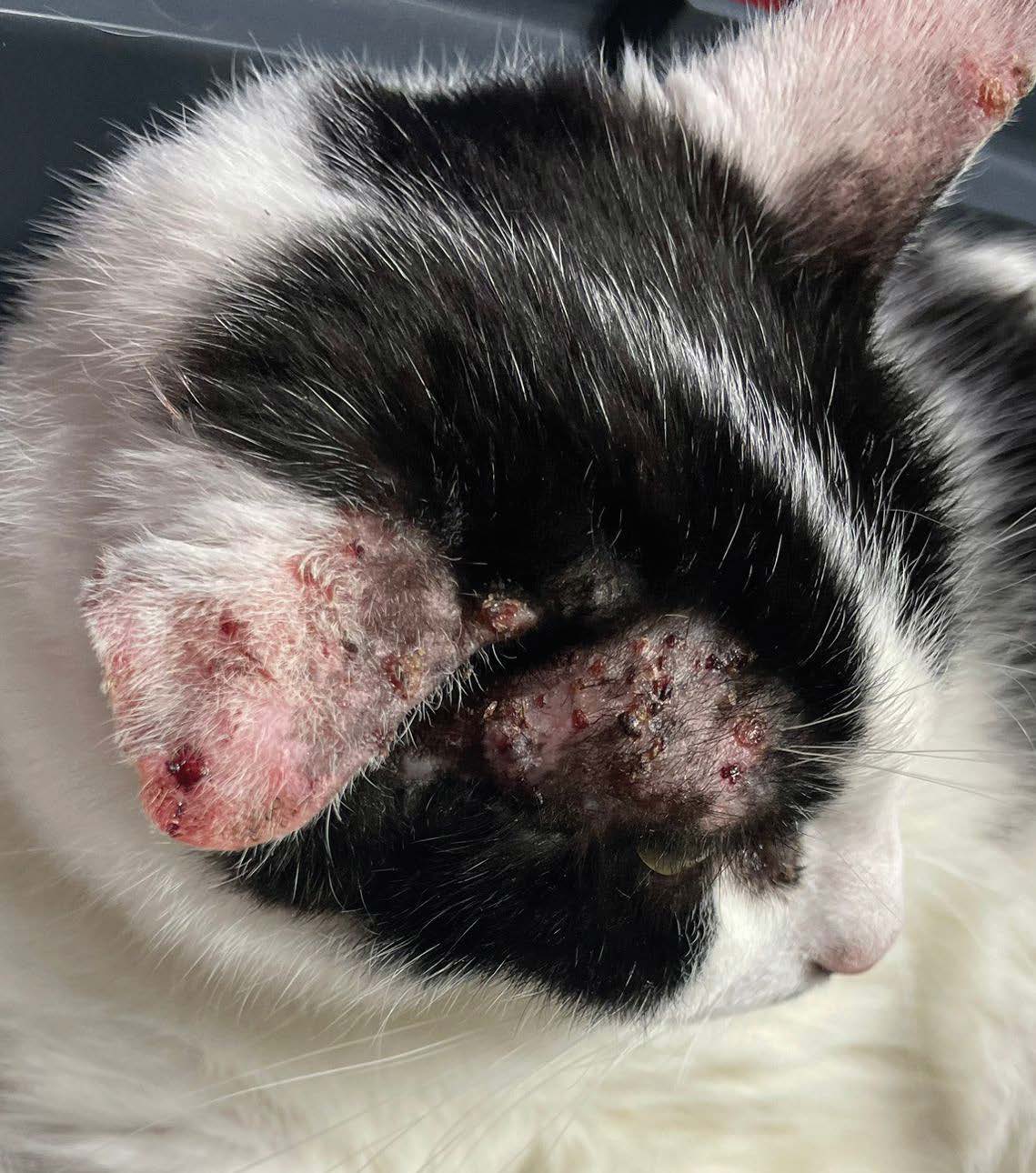
Cats are almost always (>90%) affected in the facial area (Fig. 3 and Fig. 6), around the muzzle, periocularly, and over the temples up to the ears. Crusts are often seen on the inner and outer pinnae, and in rare cases, even the ear canal is affected. Also characteristic of PF in cats are the crumbly to caseous, yellow-green coatings in the nail folds (Fig. 4) and skin changes around the mammary glands. Crusts and hyperkeratosis can also occur on the pads. However, the mucous membranes are not affected by PF. Patients with generalised skin lesions may develop fever, lethargy, anorexia, and lymph node enlargement. Immune-mediated diseases are not primarily itchy, but 25-50% of patients with PF have pruritus, which can be severe, especially with secondary bacterial or Malassezia infections.
Diagnosis
Diagnosis is based on history, clinical presentation, exclusion of differential diagnoses such as pyoderma, other immune-mediated dermatoses, dermatophytosis, demodicosis, leishmaniasis, and neoplasia (especially squamous cell carcinomas and epitheliotropic lymphomas), and finally cytological and pathohistological examination. PF can occur in all dog breeds and mixed breeds. A predisposition has been described in some breeds such as Bearded Collies, Newfoundlands, Dobermans, Spitz, and Dachshunds. Akita Inus and Chow Chows appear to be at particularly high risk of developing PF. In cats, there is no real breed predisposition; in most cases, it is the European Shorthair cat. However, in one study, Siamese cats (9%) and Ragdoll cats (6%) stood out. In our own patient population, Ragdoll cats also frequently present as PF patients.
The most important question in the history, as with all skin patients, is whether the disease was primarily itchy or whether the itching – if present – only occurred after the skin lesions. The most important differential diagnosis of PF is pyoderma, which in most cases is primarily itchy as a result of an allergy.
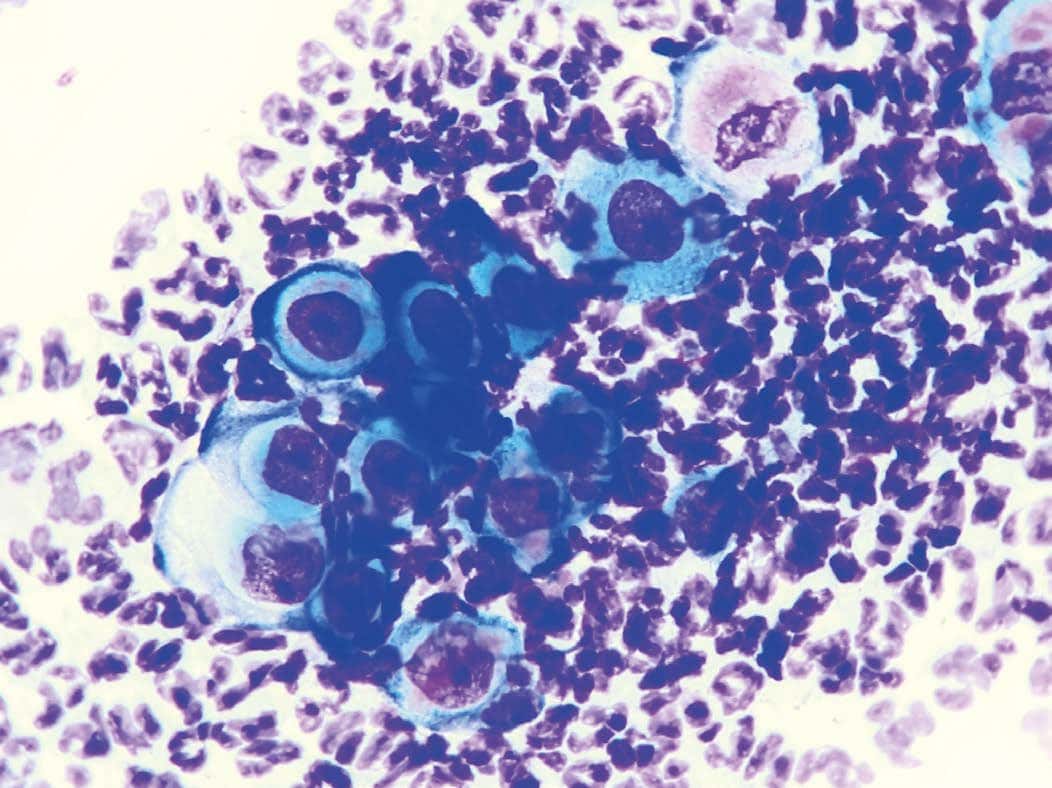
The clinical picture in cats is particularly suggestive of PF when they show classic nail fold and perimamillary changes or pustules on the inside of the ear flap. Cytology is a very important step in the diagnosis. The best material for the examination is the contents of the pustules, obtained by needle aspiration. The pustule is opened with the needle, and the exudate is smeared onto a slide or, if the amount is small, prepared by touch imprint. If no pustules are present, the underside of detached crusts and the remaining skin erosion are firmly touched to the glass slide. The cytological preparation usually shows masses of neutrophilic granulocytes in which the typical acantholytic cells are embedded (Fig. 5). These keratinocytes, which have become detached from the cell clusters, are rounded and have a darker cytoplasm than normal squamous epithelial cells, as well as a large nucleus that may also contain a nucleolus. Acantholytic cells are a clear but not pathognomonic indication of the presence of PF. They can also be found in cytological samples of chronic dermatitis of other origin.

Therefore, a pathohistological examination should always be carried out to confirm the diagnosis. In this case, the optimal material for examination is a pustule, which should ideally be removed in toto using a punch biopsy (ideally 6–8 mm). If no pustules are found in the classic locations, the next best option is to take samples from the area of thick crusts, under which acantholytic cells are usually present. If the crust detaches from the skin punch during sampling, it should definitely be placed in the sample container as well. Shaving and disinfection before the biopsy should be avoided if pemphigus foliaceus (PF) is suspected, as these procedures can damage the delicate pustules.
In the presence of secondary infection or advanced disease, clinical symptoms may be obscured, making diagnosis more difficult, with this autoimmune disease often not being included in the differential diagnoses. In such cases, cytology often shows only isolated or no acantholytic cells, in addition to inflammatory cells and microorganisms, and pathohistology may also not provide a clear result. One reason for the development of these complicated cases may be inconsistent pretreatment with antibiotics and immunosuppressive drugs when a definitive diagnosis was not made before the use of these medications. If cytological examination in these complex patients only indicates secondary infection, appropriate treatment for the bacteria or Malassezia should always be performed before obtaining samples for pathohistology. In cats, Malassezia dermatitis is almost never due to allergy alone, as it is in dogs; rather, Malassezia in this species usually indicates a more serious underlying disease process.
Therapy
The treatment of pemphigus foliaceus (PF) is based on the use of immunosuppressive drugs, either as monotherapy or, more commonly, in combination with different agents. Glucocorticoids are usually employed as the first-line treatment.
High doses are typically required in the early stages, with dexamethasone sometimes proving more effective for cats. The aim of the treatment is to achieve remission or at least a significant improvement in symptoms as quickly as possible, initially with high doses, and then to reduce the dose to the lowest level at which the patient can be kept under control (“hit hard, then back off”) to avoid side effects. If glucocorticoid monotherapy is insufficient to halt the progression of skin lesions, combination therapies with azathioprine (not for cats!), cyclophosphamide, chlorambucil, and mycophenolate mofetil are viable options. Depending on the study, cyclosporin shows varying success rates and frequent side effects; the off-label use of oclacitinib has also demonstrated varying degrees of success in the treatment of dogs and cats with PF in case reports and pilot studies. Topical preparations containing tacrolimus or glucocorticoids, such as hydrocortisone aceponate, can be used in combination with systemic therapy and sometimes even as monotherapy.

Prognosis
The prognosis for patients with pemphigus foliaceus (PF) varies greatly depending on the study; however, in general, cats have a much better prognosis (90% remission) than dogs. More recent studies indicate that treatment for dogs is also successful: 52% of dogs achieved complete remission, 35% partial remission, and only 13% were euthanised. The reasons for euthanasia in these 13% of patients included no response to treatment in only 36% of cases, unacceptable side effects in 18%, and pemphigus-unrelated or unknown circumstances in 46%. The average duration of remission in dogs is reported very differently: Almela and Chan (2021) report 4 to 7 weeks, while Mueller et al. (2006) report 7 to 12 months, depending on the treatment protocol. In cats, remission usually occurs within a month. In most patients, immunosuppressive therapy must be continued for life, as relapses are very common after complete withdrawal of the drugs. However, in studies, 2% and 12% of dogs, as well as 17% of cats, were reported to be without any relapse during the observation period after withdrawal of all medications.
Conclusion
Pemphigus foliaceus is the most commonly diagnosed autoimmune skin disease in dogs and cats. Cytology can help exclude differential diagnoses and confirm the clinical suspicion of PF; the final diagnosis is made through the pathohistological examination of punch biopsies. Immunosuppressive medications, often in combination with several drugs, are used therapeutically. Most patients respond well to the therapy, but it may take some time to achieve complete remission.
Dr Maria Christian
| Laboratory Services Relating to the Topic: |
|---|
| Cytology |
| Pathohistology |
FURTHER LITERATURE
- Almela RM, Chan T. Review of pemphigus foliaceus in dogs and cats. Today’s Veterinary Practice. November/December 2021; 11 (6): 57-68
- Bizikova P, Burrows A. Feline pemphigus foliaceus: original case series and a comprehensive literature review. BMC Vet Res. 2019; 15(1):1-15.
- Mueller RS, Krebs I, Power HT, Fieseler KV. Pemphigus foliaceus in 91 dogs. J Am Anim Hosp Assoc 2006; 42:189–196.
- Olivry T, Bergvall KE, Atlee BA. Prolonged remission after immunosuppressive therapy in six dogs with pemphigus foliaceus. Veterinary Dermatology 2004; 15: 245–52.