Pruritus, commonly known as itching, is an unpleasant sensation that provokes the reflex to scratch. Despite extensive research, the mechanisms underlying pruritus are not fully understood, making it a continued subject of investigation. Scratching, a reflexive action to alleviate itching, can temporarily relieve acute pruritus. However, in cases of chronic pruritus, this behaviour exacerbates the condition, leading to skin damage and worsening the itch-scratch cycle.
Chronic pruritus is a complex phenomenon closely related to pain. It significantly affects the quality of life for both humans and animals, often leading to insomnia, depression, agitation, and anxiety. Given these profound impacts, significant efforts are dedicated to understanding pruritus and developing effective treatments.
Types of Pruritus
Pruritus can be categorised into four types based on anatomical, physiological, and psychological factors:
1. Pruriceptive Pruritus: This type originates in the skin, triggered by sensory nerve endings responding to inflammatory mediators or skin damage. It is the most common type, associated with allergic, parasitic, or other skin disorders that
alter normal skin conditions.
2. Neuropathic Pruritus: Caused by nerve damage in peripheral or central sensory neurons, this pruritus occurs without skin-related stimuli. Examples in veterinary medicine include acral mutilation syndrome, cauda equina syndrome, and pseudorabies.
3. Neurogenic Pruritus: Unlike neuropathic pruritus, this type results from central nervous system activation without nerve damage. It is associated with systemic conditions such as liver disease or cancer and is less common in veterinary practice.
4. Psychogenic Pruritus: This type stems from psychological disorders, such as stress or depression. Diagnosed through exclusion of dermatological and neurological causes, it remains challenging to treat.
Examples include psychogenic pruritus in cats or acral lick dermatitis in dogs.
5. Chronic Pruritus: Unlike acute pruritus, chronic pruritus induces hypersensitivity in the nervous system. Peripheral sensitisation reduces activation thresholds, increasing nerve density and responsiveness. Central sensitisation alters neuronal activity, causing non-itchy stimuli to evoke itching. These changes exacerbate the itch-scratch cycle, worsening inflammation and skin damage. These phenomena highlight the need for proactive treatment to prevent escalation of clinical signs.
Assessing Pruritus in Dogs and Cats
Effective management of pruritus in dogs and cats requires an accurate assessment of it and its severity. Key steps in this process include:
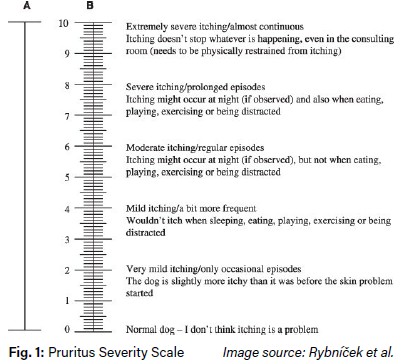
Owner Observations: Owners provide valuable insights into their animal’s condition, although these observations can be subjective. This information is gathered through anamnesis and pruritus assessment scales, with the most commonly used being the Pruritus Severity Scale by Rybníček et al. (Fig. 1).
Physical Examination: A thorough physical examination helps identify lesions indicative of pruritus. Acute pruritus may present as excoriations, erythema, hot spots, or self-induced alopecia. Chronic pruritus often manifests as lichenification, hyperpigmentation, traumatic alopecia, or eosinophilic granuloma complex lesions in cats.
Pruritus Reflexes: Evaluating reflex responses to stimuli, such as scratching or licking, helps pinpoint affected areas. Common reflexes include the pinnalpedal reflex (scratching triggered by stimulation of the auricular pinnae), the otic-pedal reflex (scratching in response to ear manipulation), and the trunk-pedal reflex.
Quality of Life Assessments: Quality of life scales assess the impact of pruritus on both the animal and its owner. These tools help evaluate how pruritus affects daily life, providing insights into the owners’ concerns and the animal’s well-being. They are also essential for making informed therapeutic decisions. Once pruritus has been identified and its severity assessed, the next step is to determine the underlying cause of the condition.

Diagnosis of Diseases Causing Pruriceptive Pruritus
Pruriceptive pruritus is the most common mechanism of pruritus in dogs and cats. Primary causes include ectoparasitic and allergic diseases. A third group consists of bacterial or Malassezia infections, which are often secondary to other skin conditions, complicating the diagnostic process. Additionally, any chronic skin disease presenting with lesions can also cause pruriceptive pruritus.
Sarcoptic Mange
• Sarcoptes Antibody Test (IgG): An ELISA test quantifies IgG antibodies in canine serum, with antibodies detectable approximately four weeks after infestation. Sensitivity is 85%, increasing to nearly 99% after four weeks of infestation, with a specificity of 90%.
• Sarcoptes PCR: Real-time PCR detects mites in extensive superficial skin scrapings from dogs, cats, ferrets, rabbits, guinea pigs, and other Canidae or Mustelidae species (reservoir: fox).
Feline demodicosis by Demodex (D.). gatoi
• PCR for D. gatoi: is postulated to be a highly effective test. As D. gatoi is not present in healthy cats, a positive result would be diagnostic. It is recommended that D. gatoi PCR be performed in all cats with pruritus before considering allergic disease.
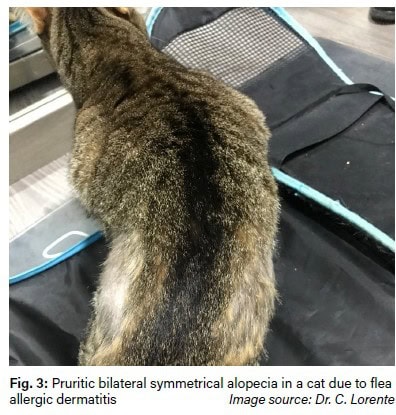
Flea Allergic Dermatitis
• Flea Saliva Antibodies: A positive result indicates hypersensitivity to flea saliva. Compatible clinical signs alongside a positive test confirm the diagnosis. The test, offered as a single IgE test (Fcε receptor), as part of an allergy screening with mites, pollens, and fungi, or within comprehensive allergy profiles by Laboklin, uses native and recombinant flea saliva allergens for high sensitivity.
Food Allergy Diagnosis
• Food allergy diagnosis requires an elimination diet for two months to control clinical signs, followed by a challenge diet to confirm recurrence. Serological food allergy testing measures allergen-specific IgE and IgG, with a negative predictive value of 81.1%. Foods without detected antibodies are suitable for elimination diets. Laboklin offers various food allergen panels, including the PAX Complete Food panel.
Atopic Dermatitis Diagnosis
• Atopic dermatitis is clinically diagnosed through detailed history and examination. Allergy tests identify causative allergens for avoidance or allergen-specific immunotherapy (ASIT) in cases of atopic dermatitis, insect hypersensitivity, or feline allergic asthma. Laboklin provides allergy panels, allergy profiles, the PAX complete environmental test, and allergen solutions for intradermal testing.
Pyoderma and Malassezia Dermatitis Diagnosis
• Cytology is the most relevant test for suspected pyoderma or Malassezia dermatitis, with Battlab providing results within 24-48 hours of sample receipt.
• Bacterial cultures identify pathogens and guide antibiotic selection. Samples must be collected under sterile conditions to prevent contamination with normal flora. Bacterial and mycological swabs should be transported in
suitable media. Antibiograms determine antimicrobial sensitivity, including MRSP identification if necessary.
Epitheliotropic Lymphoma Diagnosis
• Epitheliotropic lymphoma can present with pruritus alongside exfoliation, ulceration, depigmentation, or nodules. Histopathological examination is essential for diagnosis.
Diagnosis of Diseases Causing Neuropathic Pruritus
Some neuropathic pruritus conditions are hereditary, such as Acral Mutilation Syndrome (AMS) observed in several breeds, and Sensory Neuropathy (SN) in Border Collies. In these cases, a genetic test (PCR) is essential for confirming the diagnosis. Laboklin offers a comprehensive panel of genetic tests, including those for the aforementioned conditions.

Diagnosis of Psychogenic Pruritus
When psychogenic pruritus is suspected, it is crucial to first rule out any dermatological or internal diseases that could be causing the pruritus. Once these have been excluded, referral to a veterinary behaviour specialist (ethologist) is recommended for further assessment and management.
Treatment of Pruritus
The treatment of pruritus is essential from the very first moment, aiming to relieve clinical signs and improve the animal’s condition. In cases of severe pruritus, treatment should begin even while investigating the underlying cause.
Treatment approaches include both reactive and proactive strategies:
• Reactive Treatment: controls pruritus during acute phases of disease.
• Proactive Treatment: maintains control after resolving acute signs, preventing relapses in conditions like atopic dermatitis.
Systemic Treatment Options
• Glucocorticoids: These anti-inflammatory drugs are effective and fast-acting but should be used cautiously to avoid side effects. Commonly used are oral prednisolone or prednisone, with dosages tailored to individual needs.
• Oclacitinib (Apoquel®): A JAK-STAT inhibitor that targets IL-31, providing rapid relief for allergic pruritus. It is safer than glucocorticoids and particularly effective for atopic dermatitis in dogs.
• Lokivetmab: This monoclonal antibody neutralizes IL-31 and is administered subcutaneously every four weeks. It is a safe and effective option for proactive management of atopic dermatitis.
• Cyclosporin: An immunosuppressant that inhibits calcineurin, cyclosporine is ideal for long-term management of allergic conditions. It requires an initial loading dose followed by maintenance therapy and can be combined with other treatments during flare-ups.
Conclusion
Pruritus, whether acute or chronic, demands effective management to alleviate suffering and improve quality of life. Identifying and treating the disease is essential for long-term success. Collaboration between general practitioners and specialists ensures optimal care, providing relief for affected animals and their owners alike.
Dr. Carmen Lorente, DVM, PhD, DipECVD
EBVS® European Specialist in Veterinary Dermatology
Services on the topic
- Pruritus Profile small/medium/large
- Allergy pre-test and main tests
- PAX complete (environmental allergens, feed)
- Flea Saliva, Sarcoptes Ab, Malassezia Ab, Staphylococcus Ab
- Demodex-PCR, Sarcoptes-PCR